cancer immunotherapy: Optimal Treatment Solutions
Cancer immunotherapy has emerged as a revolutionary approach in the field of cancer treatment. Unlike traditional treatments that target the cancer cells directly, immunotherapy harnesses the body’s immune system to recognize and destroy cancer cells. This article dives into the world of cancer immunotherapy, exploring its different approaches, benefits, challenges, and potential for transforming the landscape of cancer care.
The Basis of Cancer Immunotherapy
What is Cancer Immunotherapy?
Cancer immunotherapy, also known as immuno-oncology, is a groundbreaking treatment that enhances the body’s natural defense mechanisms against cancer. It works by stimulating the immune system to identify and attack cancer cells as foreign invaders.
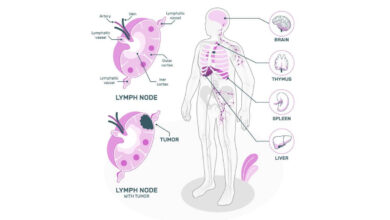
The Role of Immune Cells
Key immune cells, such as T cells and natural killer cells, play a pivotal role in cancer immunotherapy. These cells are trained to recognize specific molecules present on the surface of cancer cells, initiating an immune response to eliminate them.
Types of Cancer Immunotherapy
Checkpoint Inhibitors
Checkpoint inhibitors are a common form of immunotherapy that target proteins on immune cells or cancer cells, preventing them from inhibiting immune responses. This unleashes the immune system to effectively combat cancer.
Cancer Vaccines
Cancer vaccines contain antigens that stimulate the immune system to recognize and remember cancer cells. This approach helps the immune system respond more vigorously if cancer reoccurs.
Adoptive T Cell Therapy
Adoptive T cell therapy involves extracting, modifying, and multiplying T cells outside the body before infusing them back. These modified T cells can then better target and destroy cancer cells.
Advantages of Cancer Immunotherapy
Targeted Treatment
Immunotherapy’s precision targeting reduces damage to healthy cells, leading to fewer side effects compared to traditional treatments like chemotherapy.
Long-Term Response
Some patients experience long-lasting responses to immunotherapy, with their immune system effectively controlling cancer growth for extended periods.
Potential for Combining Therapies
Immunotherapy can be combined with other treatments like chemotherapy or radiation therapy to create a synergistic effect, enhancing overall treatment outcomes.
Challenges and Considerations
Immune Resistance
In some cases, cancer cells develop mechanisms to evade the immune system, limiting the effectiveness of immunotherapy. Researchers are actively working to overcome this challenge.
Personalized Approach
Cancer immunotherapy’s success may vary based on an individual’s immune response, requiring personalized treatment plans.
Side Effects
While immunotherapy has fewer side effects, some patients may still experience immune-related reactions that need careful management.
The Future of Cancer Immunotherapy
Expanding Research
Ongoing research aims to broaden the range of cancers treatable with immunotherapy and enhance its effectiveness.
Targeting Rare Cancers
Immunotherapy shows promise in treating rare cancers that lack targeted treatment options.
Immunotherapy and Precision Medicine
The integration of immunotherapy into precision medicine approaches holds potential for tailoring treatment to an individual’s unique genetic makeup.
Cancer immunotherapy represents a paradigm shift in cancer treatment, offering hope to patients by harnessing the body’s own defenses. As research advances, this approach will likely continue to reshape the way we approach and manage cancer.
How Does Immunotherapy Work Against Cancer?
- Activating the Immune Response
At the core of immunotherapy’s effectiveness lies its ability to activate and enhance the body’s immune response. The immune system is equipped with specialized cells, including T cells and natural killer cells, which are responsible for identifying and neutralizing abnormal or foreign cells, including cancer cells.
- Overcoming Immune Evasion
Cancer cells often employ various tactics to evade detection by the immune system. Immunotherapy disrupts these evasive mechanisms. One prominent example is the use of checkpoint inhibitors. Checkpoints are proteins that prevent immune cells from attacking healthy cells, but cancer cells can exploit these checkpoints to avoid detection. Checkpoint inhibitor drugs block these proteins, freeing the immune system to target and destroy cancer cells.
- Targeting Cancer-Specific Antigens
Immunotherapy takes advantage of the fact that cancer cells express unique antigens, or surface markers, that distinguish them from normal cells. Researchers develop vaccines or therapies that expose the immune system to these antigens, effectively training it to recognize and attack cancer cells.
- Adoptive T Cell Therapy
Adoptive T cell therapy involves extracting T cells from a patient’s body and genetically modifying them to express receptors that can target cancer cells. These modified T cells are then multiplied in the lab before being infused back into the patient. Once inside the body, they recognize and attack cancer cells with precision.
- Amplifying Immune Memory
Immunotherapy not only targets existing cancer cells but also enhances the immune system’s memory. This means that if cancer were to recur, the immune system would recognize it more quickly and respond more effectively, preventing relapse.
Types of Cancer Immunotherapy
There are several approaches to cancer immunotherapy:
Checkpoint Inhibitors
As mentioned earlier, checkpoint inhibitors are drugs that block proteins that hinder immune responses. By inhibiting these checkpoints, the immune system can target and destroy cancer cells.
Immune Checkpoint Modulators
These drugs modulate immune responses, enhancing the body’s ability to recognize and fight cancer cells.
Monoclonal Antibodies
Monoclonal antibodies are designed to recognize specific cancer cells and mark them for destruction by immune cells.
Considerations and Challenges
While immunotherapy offers promising results, it’s not a universal cure. Factors such as the type of cancer, individual patient responses, and potential side effects need to be carefully considered.
Immunotherapy’s ability to mobilize the immune system against cancer represents a revolutionary step forward in cancer treatment. By leveraging the body’s natural defenses, immunotherapy offers hope for more targeted, less toxic, and potentially more effective cancer therapies.
Which cancers are treated with immunotherapy?
Melanoma Skin Cancer
One of the earliest success stories of immunotherapy is in the treatment of melanoma, a type of skin cancer. Immune checkpoint inhibitors have shown remarkable efficacy in patients with advanced melanoma by boosting the immune response against cancer cells.
Lung Cancer
Immunotherapy has brought new hope to lung cancer patients, particularly those with non-small cell lung cancer. Checkpoint inhibitors have demonstrated significant improvements in survival rates and disease progression compared to traditional treatments.
Kidney Cancer
Certain types of kidney cancers, such as renal cell carcinoma, have responded positively to immunotherapy. Immune checkpoint inhibitors have proven effective in shrinking tumors and extending survival in patients with advanced kidney cancer.
Bladder Cancer
Immunotherapy has revolutionized the treatment landscape for bladder cancer. Checkpoint inhibitors have shown substantial benefits, especially for patients who have not responded to standard chemotherapy.
Lymphoma
Lymphomas, including both Hodgkin and non-Hodgkin types, have shown promising responses to immunotherapy. Monoclonal antibodies have been used to specifically target lymphoma cells, enhancing treatment outcomes.
Leukemia
Immunotherapy is also making strides in the treatment of leukemia. CAR-T cell therapy, a form of adoptive T cell therapy, has shown remarkable success in treating certain types of leukemia by engineering T cells to target cancer cells.
Head and Neck Cancers
Immunotherapy has demonstrated potential in treating head and neck cancers, particularly in cases where other treatments have not been effective. Checkpoint inhibitors have shown promise in improving survival rates and quality of life.
Colorectal Cancer
While traditionally considered challenging to treat with immunotherapy, advancements are being made in using checkpoint inhibitors to target specific genetic mutations in colorectal cancer cells.
Liver Cancer
Liver cancer, including hepatocellular carcinoma, is being explored for immunotherapy treatments. Clinical trials are investigating the potential benefits of combining immunotherapy with other treatment modalities.
Immunotherapy’s impact on cancer treatment extends to a diverse array of cancer types. As research and development continue, the hope is that immunotherapy will become an integral part of the oncology toolkit, offering new avenues of hope for patients across the cancer spectrum.
What are the side effects of immunotherapy?
Immune-Related Adverse Events
Immunotherapy works by enhancing the immune system’s activity, which can sometimes lead to immune-related adverse events. These side effects occur when the immune system attacks healthy tissues in addition to cancer cells.
Skin Reactions
Skin reactions are common side effects of immunotherapy. Patients may experience rashes, itching, or blistering. In some cases, autoimmune conditions like dermatitis or vitiligo, which cause skin discoloration, can also occur.
Gastrointestinal Issues
Gastrointestinal side effects are also possible. Patients may experience diarrhea, nausea, vomiting, or even inflammation of the intestines (colitis). These symptoms can range from mild to severe.
Fatigue
Fatigue is a frequent complaint among patients undergoing immunotherapy. While the exact cause is not fully understood, it’s believed to be related to the immune system’s heightened activity.
Endocrine Dysfunction
Immunotherapy can disrupt the normal functioning of the endocrine system, leading to hormonal imbalances. Conditions like hypothyroidism or hyperthyroidism may develop.
Respiratory Issues
In some cases, immunotherapy-related lung inflammation, known as pneumonitis, can occur. Patients may experience symptoms such as shortness of breath and coughing.
Liver Inflammation
Immunotherapy can lead to inflammation of the liver, known as hepatitis. Monitoring liver function is essential during treatment.
Management and Prevention
To manage and prevent side effects, communication between patients and healthcare providers is crucial. Regular check-ups and open discussions about symptoms can lead to timely interventions.
Immune-Related Adverse Events Grading
Side effects are often graded based on severity. Grade 1 refers to mild symptoms, while grade 4 indicates life-threatening reactions. Prompt reporting of symptoms helps determine appropriate management strategies.
Treatment Interruptions and Modifications
In some cases, treatment may need to be temporarily interrupted or modified to allow the body to recover from side effects. Once symptoms are under control, treatment can be resumed.
While immunotherapy offers significant benefits in cancer treatment, it’s essential to be aware of potential side effects. Open communication with healthcare providers and early intervention can ensure that side effects are managed effectively, allowing patients to continue their journey towards better health.
How is immunotherapy given?
Intravenous (IV) Infusion
One of the most common methods of delivering immunotherapy is through intravenous (IV) infusion. Medications such as immune checkpoint inhibitors, monoclonal antibodies, and adoptive T cell therapies are often administered directly into the bloodstream. IV infusion allows the medication to circulate throughout the body, targeting cancer cells wherever they may be located.
Subcutaneous Injections
Some immunotherapy drugs, particularly vaccines and certain checkpoint inhibitors, can be administered through subcutaneous injections. These injections are delivered into the fatty tissue just beneath the skin. Subcutaneous administration is convenient and often preferred by patients who may require frequent doses.
Oral Medications
Certain types of immunotherapy drugs, such as targeted therapies and immune modulators, can be taken orally in the form of pills or capsules. Oral medications offer convenience and can be taken at home, reducing the need for frequent hospital visits.
Intratumoral Injections
For some types of immunotherapy, such as oncolytic viruses or certain cytokines, medications are injected directly into the tumor itself. These intratumoral injections aim to stimulate a local immune response and promote the destruction of cancer cells within the tumor.
CAR-T Cell Therapy
CAR-T cell therapy involves a more intricate process. T cells are extracted from the patient’s blood and then genetically modified in a lab to express chimeric antigen receptors (CARs) that target cancer cells. These modified T cells are then infused back into the patient’s bloodstream to seek out and destroy cancer cells.
Intralesional Therapy
Intralesional therapy involves injecting immunotherapy drugs directly into specific lesions or tumors. This approach is commonly used for skin cancers and is particularly effective in cases where the tumor is easily accessible.
Combination Therapies
Immunotherapy can also be administered in combination with other treatments, such as chemotherapy or radiation therapy. This approach, known as combination therapy, aims to enhance the overall effectiveness of treatment by targeting cancer cells through multiple mechanisms.
The diverse delivery methods of immunotherapy underscore its versatility and potential to address a wide range of cancers. The choice of administration method depends on factors such as the type of immunotherapy, the specific cancer being treated, and the patient’s overall health. As research continues, new and innovative delivery methods are likely to emerge, further expanding the horizons of cancer treatment.
How often do you receive immunotherapy?
Treatment Type and Regimen
The frequency of immunotherapy sessions depends on the specific treatment type and regimen recommended by your healthcare provider. Some treatments involve receiving immunotherapy drugs over a set period, while others may require ongoing or intermittent therapy.
Drug Administration Method
The method of drug administration plays a significant role in determining treatment frequency. Immunotherapy can be delivered through intravenous (IV) infusions, subcutaneous injections, or oral medications. IV infusions are typically administered over a few hours and may occur every few weeks or months, while oral medications might be taken daily, weekly, or as directed.
Treatment Goals
The goals of immunotherapy influence treatment frequency. Some patients may receive immunotherapy with the intent of achieving remission or controlling disease progression. In such cases, treatment frequency may be more intensive initially and then gradually spaced out as treatment goals are met.
Response to Treatment
Your response to immunotherapy also affects the treatment schedule. If you respond well and experience positive outcomes, your healthcare provider might adjust the treatment frequency to maintain the benefits and manage any potential side effects.
Clinical Trials
If you’re participating in a clinical trial exploring new immunotherapy approaches, the treatment schedule may follow the trial protocol. Clinical trials often involve closely monitored and structured treatment plans that can influence the frequency of sessions.
Personalized Treatment Plans
Every patient’s treatment plan is tailored to their individual needs and circumstances. Your healthcare provider will take into account factors such as your overall health, cancer type, stage, and response to treatment when determining the optimal treatment schedule.
Follow-Up Appointments
In addition to treatment sessions, follow-up appointments are essential for monitoring your progress and adjusting your treatment plan as needed. These appointments allow your healthcare provider to assess how well the immunotherapy is working and make any necessary modifications.
The frequency of immunotherapy sessions varies widely based on several factors, including the type of immunotherapy, your individual treatment plan, and your body’s response to the treatment. It’s important to communicate openly with your healthcare provider and adhere to the recommended treatment schedule to achieve the best possible outcomes in your cancer journey.
How can you tell if immunotherapy is working?
Imaging Scans
Imaging scans, such as CT scans, MRI, or PET scans, play a vital role in monitoring the response to immunotherapy. These scans provide detailed images of the body’s internal structures and can show changes in tumor size, shape, and activity over time.
Tumor Markers
Tumor markers are substances that can be measured in the blood and indicate the presence of cancer. Monitoring changes in tumor marker levels can provide insights into how well immunotherapy is affecting the cancer.
Clinical Examinations
Regular clinical examinations by your healthcare provider are essential for assessing the physical response to immunotherapy. These examinations can help detect changes in the tumor’s size, consistency, or appearance.
Biopsies
Biopsies involve taking a sample of tissue from the tumor and analyzing it under a microscope. Changes in the tumor’s composition, such as reduced cell activity or increased immune cell infiltration, can indicate a positive response to immunotherapy.
Response Evaluation Criteria
Response Evaluation Criteria, such as RECIST (Response Evaluation Criteria in Solid Tumors) or irRECIST (immune-related RECIST), are standardized guidelines used to assess tumor response to treatment. These criteria categorize responses as complete response, partial response, stable disease, or progressive disease.
Duration of Response
The duration of the response is a critical indicator of immunotherapy’s effectiveness. Prolonged periods of stable disease or regression suggest a positive response to treatment.
Quality of Life
Improvements in your overall quality of life can also signal that immunotherapy is working. If you experience fewer symptoms, increased energy, and enhanced well-being, it indicates a positive impact on your health.
Communication with Healthcare Provider
Regular communication with your healthcare provider is essential for tracking your progress. They can interpret the results of tests, scans, and examinations and provide insights into how well the immunotherapy is working.
Combination Therapies
In some cases, immunotherapy may be combined with other treatments like chemotherapy or targeted therapies. Positive outcomes from combination therapies can also indicate the effectiveness of immunotherapy.
Assessing the effectiveness of immunotherapy requires a combination of medical evaluations, imaging techniques, and communication with your healthcare provider. It’s important to remember that response to immunotherapy can vary among individuals, and results may not be immediate. Close monitoring and collaboration with your healthcare team will help determine if the treatment is achieving the desired outcomes in your cancer journey.
What is the current research in immunotherapy?
Personalized Immunotherapy
Researchers are increasingly focusing on developing personalized immunotherapy approaches tailored to each patient’s unique genetic makeup, immune system characteristics, and cancer type. Personalized vaccines and targeted therapies are being explored to enhance treatment effectiveness and minimize side effects.
Neoantigens and Cancer Vaccines
Neoantigens are unique markers present on cancer cells but not on normal cells. These antigens are attractive targets for immunotherapy. Cancer vaccines that expose the immune system to neoantigens are being developed to stimulate a robust and targeted immune response against cancer cells.
Combination Therapies
Combining different immunotherapy approaches, as well as immunotherapy with other treatment modalities like chemotherapy or radiation, is a growing area of research. Combination therapies aim to create synergistic effects that enhance the immune response and improve treatment outcomes.
Overcoming Immunotherapy Resistance
While immunotherapy has shown remarkable success, some patients develop resistance to treatment. Researchers are investigating ways to overcome this resistance by understanding the mechanisms that allow cancer cells to evade the immune system and developing strategies to counteract them.
Biomarkers for Response Prediction
Identifying biomarkers that can predict a patient’s response to immunotherapy is a crucial focus. Researchers are studying genetic, molecular, and immune system factors that can help determine who is likely to benefit from immunotherapy and tailor treatment plans accordingly.
Microbiome and Immunotherapy
Recent research suggests that the gut microbiome plays a significant role in modulating the immune response. Studies are exploring how the gut microbiome influences immunotherapy outcomes and whether manipulating the microbiome can enhance treatment efficacy.
Cell Therapy Advancements
Cell-based therapies like CAR-T cell therapy continue to advance. Researchers are exploring ways to improve the efficiency and safety of these therapies, expand their application to different cancer types, and overcome challenges like immune-related toxicities.
Targeting Rare Cancers
Immunotherapy is showing promise in treating rare and hard-to-treat cancers that lack effective targeted treatments. Research efforts are focused on developing immunotherapies specifically tailored to these rare cancer types.
Enhancing Memory Response
Developing immunotherapies that create a lasting memory response within the immune system is a key goal. This memory response ensures that the immune system can recognize and respond to cancer cells if they reappear.
The landscape of immunotherapy research is vibrant and rapidly evolving, with researchers continually pushing the boundaries of knowledge and innovation. These trends highlight the ongoing commitment to improving cancer treatment, offering renewed hope for patients and shaping the future of oncology.
Frequently Asked Questions
- Who is eligible for cancer immunotherapy?
Cancer immunotherapy may be considered for various cancer types and stages. Consultation with a medical professional is essential to determine eligibility.
- Is immunotherapy a standalone treatment?
Immunotherapy can be used alone or in combination with other treatments, depending on the specific case and cancer type.
- Are there potential side effects of immunotherapy?
While generally milder than traditional treatments, immunotherapy can still lead to immune-related side effects that require monitoring and management.
- How long does an immunotherapy treatment course last?
The duration of treatment varies based on the patient’s response and the specific immunotherapy approach used.
- Is cancer immunotherapy covered by insurance?
Coverage depends on the insurance provider and policy. It’s advisable to verify coverage options before starting treatment.