Rheumatoid arthritis (RA) is a formidable adversary, stealthily infiltrating the body’s defenses and wreaking havoc on joints, organs, and overall well-being. In this comprehensive article, we delve into the intricate tapestry of RA, exploring its genetic roots, clinical manifestations, diagnostic challenges, and the evolving landscape of therapeutic interventions.
Understanding the Basics
1. What Is Rheumatoid Arthritis?
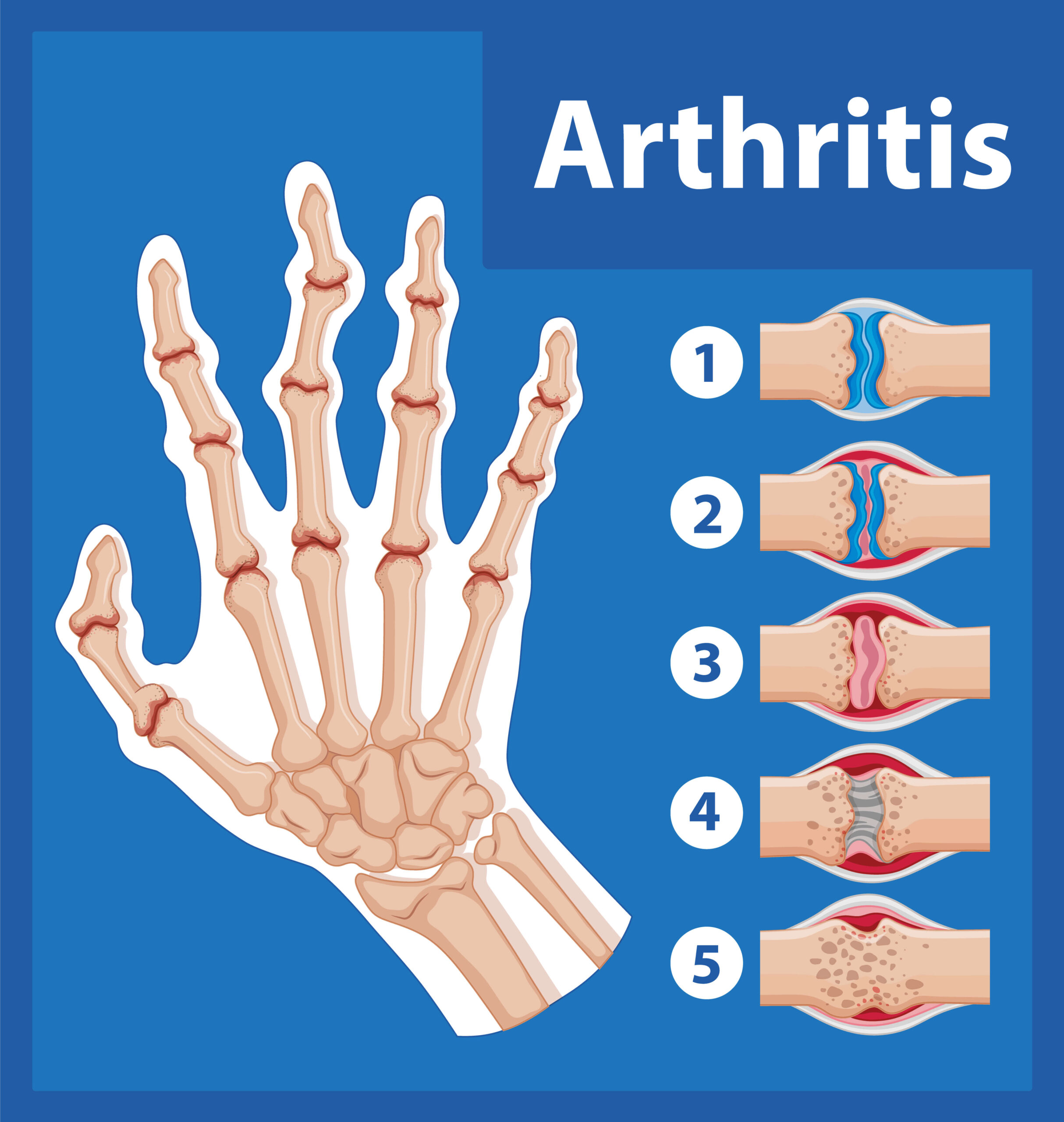
RA is an autoimmune inflammatory disease that primarily targets the synovial lining of joints. Unlike the wear-and-tear arthritis (osteoarthritis), which results from mechanical stress, RA arises from the immune system’s misguided assault on healthy tissues. The hallmark feature is synovitis—swelling, pain, and stiffness in multiple joints. But RA doesn’t stop there; it can also affect other organs, leading to complications such as interstitial pneumonia, cardiovascular issues, and ocular inflammation.
2. The Genetic Predisposition
While environmental factors play a role, genetics significantly influence RA susceptibility. Certain human leukocyte antigen (HLA) genes, particularly HLA-DRB1, are strongly associated with RA risk. These genes shape the immune response, determining whether the body tolerates or attacks its own tissues. Additionally, non-HLA genes contribute to the complex genetic landscape of RA.
3. Clinical Presentation
RA often strikes women between their 30s and 50s, although it can affect anyone. The classic triad of symptoms includes joint pain, swelling, and morning stiffness. The joints—typically small ones like those in the hands and feet—become tender and warm. Over time, joint destruction ensues, leading to deformities and irreversible physical limitations.
4. Diagnosis Dilemmas
Early diagnosis is crucial for effective management. However, RA masquerades as other conditions, making diagnosis challenging. Rheumatologists rely on a combination of clinical assessment, blood tests (such as rheumatoid factor and anti-cyclic citrullinated peptide antibodies), and imaging (X-rays, ultrasound, or MRI) to confirm RA.
Navigating Treatment Options
1. Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs form the cornerstone of RA treatment. These drugs suppress the immune system’s aberrant activity, aiming to halt disease progression. They fall into three categories:
- Conventional Synthetic DMARDs: Methotrexate, sulfasalazine, and hydroxychloroquine are examples. They reduce inflammation and prevent joint damage.
- Targeted Synthetic DMARDs: Janus kinase (JAK) inhibitors like tofacitinib belong here. They selectively inhibit specific pathways involved in RA.
- Biologic DMARDs: Monoclonal antibodies (such as adalimumab, rituximab, and tocilizumab) target specific immune molecules. Biologics revolutionized RA management.
2. Precision Medicine and Beyond
The era of personalized medicine beckons. Researchers explore genetic variations that predict treatment response. Tailoring therapy based on an individual’s genetic makeup could optimize outcomes. Moreover, drug holidays and curative strategies are on the horizon.
3. Hope Amidst Challenges
RA remains a formidable adversary, but advances in understanding its pathogenesis and targeted therapies offer hope. By maintaining remission and preventing joint destruction, we inch closer to a future where RA’s grip loosens, allowing patients to reclaim their lives.
Read also about Living a Healthy Lifestyle: Vitality and Longevity Tips
Conclusion
As we unravel the mysteries of RA, we honor centuries of medical progress. From ancient willow bark remedies to cutting-edge biologics, our journey continues. Let us champion research, empathy, and resilience in the fight against this relentless foe.