Testicular cancer is a type of cancer that develops in the testicles, which are the male reproductive organs responsible for producing sperm and testosterone. While testicular cancer is a serious condition, it is also one of the most curable forms of cancer, with a high survival rate.
One of the concerns that men with testicular cancer may have is whether they can father children after treatment. Testicular cancer and its treatments can affect a man’s fertility, but there are options available to preserve or restore fertility. In this article, we will explore the relationship between testicular cancer and fertility, and what men can do to increase their chances of fathering children.
Understanding the Link between Testicular Cancer and Fertility:
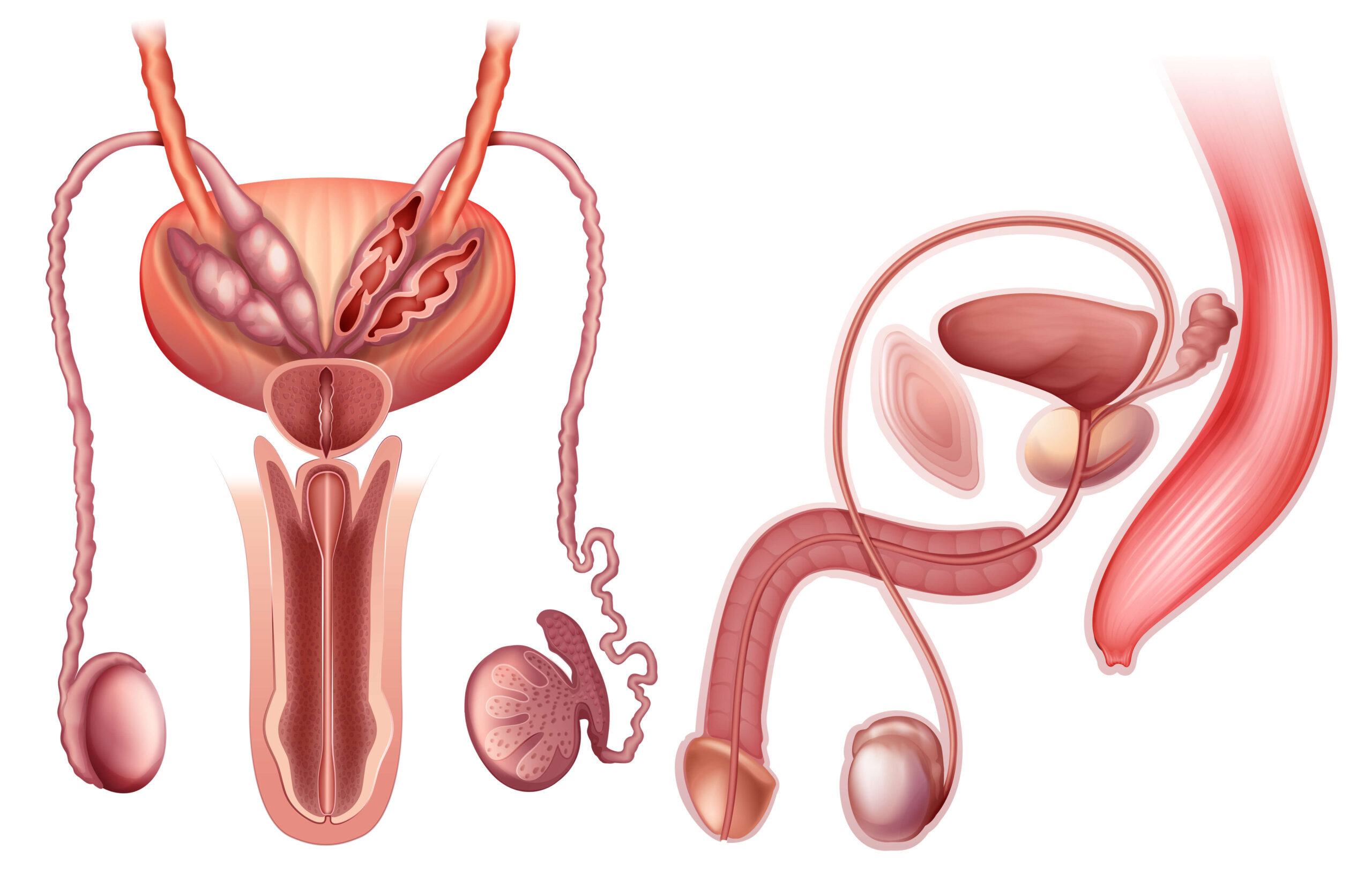
Testicular cancer and its treatments can have a significant impact on a man’s fertility. The testicles produce sperm, which are necessary for fertilization and conception. Testicular cancer can damage the testicles, and treatments like chemotherapy and radiation therapy can also affect sperm production and quality.
Chemotherapy drugs can damage sperm cells and cause low sperm counts, which can make it difficult to father children. Radiation therapy can also damage the testicles and reduce sperm production. In some cases, radiation therapy can also cause permanent infertility.
The impact of testicular cancer and its treatments on fertility depends on several factors, including the type of cancer, the stage of the cancer, and the treatment used. Men who undergo surgery to remove a testicle may still be able to father children with the remaining testicle, but their fertility may be reduced. In cases where both testicles are removed, the man will be infertile.
Options for Preserving Fertility:
For men who want to father children after testicular cancer treatment, there are several options available to preserve fertility before treatment. These options include sperm banking, testicular sperm extraction (TESE), and testicular tissue banking.
Sperm banking involves collecting and freezing sperm before treatment, which can be used for fertility treatments like in vitro fertilization (IVF) after treatment. Sperm banking is the most common option for preserving fertility in men with testicular cancer, and it is recommended for all men who may want to father children in the future.
TESE involves extracting sperm directly from the testicle. This procedure is typically done under local anesthesia and involves removing small samples of testicular tissue to search for sperm. If sperm are found, they can be frozen for use in fertility treatments.
Testicular tissue banking involves freezing a small piece of testicular tissue before treatment. This tissue can later be used to extract sperm for use in fertility treatments.
Options for Restoring Fertility:
In cases where testicular cancer treatment has resulted in infertility, there are options available to restore fertility. These options include sperm retrieval, IVF, and intracytoplasmic sperm injection (ICSI).
Sperm retrieval involves extracting sperm directly from the testicle or epididymis using a needle. This procedure can be done under local anesthesia and is typically a simple and quick procedure. The retrieved sperm can then be used for fertility treatments like IVF or ICSI.
IVF involves fertilizing an egg with sperm in a laboratory and then transferring the resulting embryo to the uterus. ICSI is a form of IVF that involves injecting a single sperm directly into an egg. This can be helpful in cases where the sperm count is very low.
In some cases, men with testicular cancer may also be candidates for testicular prosthesis. This involves implanting a synthetic testicle to replace a removed testicle. While a testicular prosthesis does not restore fertility, it can help with self-esteem and body image issues.
While sperm banking is the most common and effective option for preserving fertility, it is not always an option for every man. Men who have already undergone treatment or who have a low sperm count may need to consider other options for restoring fertility, such as sperm retrieval and IVF.
It is also important to note that fertility treatments like IVF can be expensive and may not always result in a successful pregnancy. Men and their partners should discuss their options and expectations with a fertility specialist to determine the best course of action.
How does testicular cancer cause infertility?
Testicular cancer can cause infertility by damaging the testicles, which are the male reproductive organs responsible for producing sperm. The cancer cells can grow and invade the healthy tissues of the testicles, which can affect the production and quality of sperm.
Additionally, the treatments used to treat testicular cancer, such as chemotherapy and radiation therapy, can also affect fertility. Chemotherapy drugs can damage sperm cells and cause low sperm counts, which can make it difficult to father children. Radiation therapy can also damage the testicles and reduce sperm production. In some cases, radiation therapy can cause permanent infertility.
The impact of testicular cancer and its treatments on fertility depends on several factors, including the type of cancer, the stage of the cancer, and the treatment used. Men who undergo surgery to remove a testicle may still be able to father children with the remaining testicle, but their fertility may be reduced. In cases where both testicles are removed, the man will be infertile.
It is important for men with testicular cancer to discuss their fertility concerns with their healthcare provider and explore their options for preserving or restoring fertility before treatment. Sperm banking, testicular sperm extraction (TESE), and testicular tissue banking are all options available to preserve fertility before treatment. Sperm retrieval, in vitro fertilization (IVF), and intracytoplasmic sperm injection (ICSI) are options for restoring fertility after treatment.
Can testicular cancer cause birth defects?
There is no evidence to suggest that testicular cancer itself can cause birth defects in children. However, the treatments used to treat testicular cancer, such as chemotherapy and radiation therapy, may increase the risk of birth defects.
Chemotherapy drugs can cross the placenta and affect the developing fetus. Some chemotherapy drugs have been linked to an increased risk of birth defects, particularly when given during the first trimester of pregnancy. The risk of birth defects may also be higher if chemotherapy is given in combination with other treatments, such as radiation therapy.
Radiation therapy can also affect the developing fetus and increase the risk of birth defects. The risk of birth defects depends on the dose of radiation and the stage of fetal development at the time of exposure. Radiation therapy is usually avoided during pregnancy if possible.
For men who are planning to have children after treatment for testicular cancer, it is important to discuss their fertility concerns and the potential risks of birth defects with their healthcare provider. Men may need to delay conception until after treatment or use assisted reproductive technologies, such as IVF with preimplantation genetic diagnosis (PGD), to reduce the risk of birth defects.
while testicular cancer itself does not appear to cause birth defects, the treatments used to treat the cancer can increase the risk. It is important for men with testicular cancer to discuss their options for preserving fertility and the potential risks with their healthcare provider before undergoing treatment.
In conclusion, men with testicular cancer can still father children after treatment, but it may require planning and intervention. Preserving fertility through sperm banking or other methods can increase the chances of a successful pregnancy in the future. Men who have undergone treatment and are experiencing infertility can also explore options for restoring fertility, such as sperm retrieval and IVF. It is important for men with testicular cancer to discuss their fertility concerns with their healthcare provider and explore their options before treatment to increase their chances of fathering children in the future.